HIV’s secret sweet tooth: T cell glycosylation determines variant entry
From the Overbaugh Lab, Human Biology and Public Health Sciences Divisions
November 22, 2024 | By Jenny Waters
At the cellular level, HIV-1 transmission involves a highly coordinated process whereby the virus binds to CD4 receptors and one of two coreceptors—CCR5 (R5) or CXCR4 (X4)—on host immune cells, enabling viral entry. R5-prefering HIV-1 strains are typically dominant in early infection, while tropic switching from R5- to X4-specific HIV-1 typically occurs in the later stages of infection as mutations in the virus allow it to shift its coreceptor usage. This switch is associated with a faster decline in CD4+ T cells and accelerated disease progression, as nearly all CD4 T cells express CXCR4 compared to 15-30% which express CCR5, enabling X4-tropic viruses to target a broader range of T cells.
The prevalence of R5 viruses in early infection stems from a phenomenon called a “population bottleneck,” which can be compared to planting seeds in a new garden. When you plant only a few seeds, not every type can thrive right away—only the ones best suited to the soil will take root initially. Similarly, in HIV transmission, R5-tropic HIV variants are able to "take root" in a new host better than their X4-tropic counterparts. Over time, as the conditions of the immune system evolve, other "seeds" (or viral types, like X4) may also find favorable conditions and start to grow. In a recent study published in Nature Microbiology, researchers from Julie Overbaugh’s lab in the Human Biology division have unraveled some of the mysteries surrounding preferential transmission of R5 HIV-1.
“Our study aimed to better understand why some HIV-1 strains are more transmissible than others,” begins Dr. Hannah Itell, a former graduate student in the Overbaugh lab. To accomplish this goal, Itell and colleagues designed a CRISPR screen to interrogate the importance of 2000 candidate host genes in infection of primary T cells by either an R5 or an X4 HIV virus. Using this sophisticated screening strategy, they discovered 81 genes which specifically suppress X4-tropic HIV viruses but not R5-tropic ones—they termed these genes X4-tropic “restriction factors”. Restriction factors are proteins that prevent viruses from replicating inside a host and often make up the first line of defense against viral infection. Focusing on one of these genes, Itell states “We identified a host protein called SLC35A2 that impacts HIV-1 infection based on what coreceptor the given viral strain uses. SLC35A2 expression promotes R5 infection while hindering that of X4 viruses—the same trend that we know exists during HIV-1 transmission.”
So, how is SLC35A2 expression selecting for R5 infection? As it turns out, the answer lies in a process called glycosylation—the attachment of specific sugar molecules to proteins or fats. In the spirit of the approaching holiday season, think of this like decorating a tree with ornaments: these sugars are added onto proteins and lipids to help them work properly. This “decorating” helps a protein fold into the right shape, move to the correct part of the cell, or interact with other molecules. SLC35A2 specifically encodes a protein that attaches the sugar galactose to other proteins, and the effect of SLC35A2 knockout on glycosylation can therefore be measured by staining cells for two glycan-binding lectins (GSL-II and VVL, proteins that bind to carbohydrates)that would only be exposed in cells lacking galactose. By staining for GSL-II and VVL, Itell was able to show that SLC35A2 loss-of-function does in fact result in truncated cell-surface glycans.
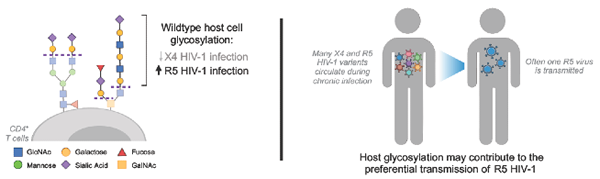
A “population bottleneck” occurs during HIV-1 transmission – despite numerous X4 and R5 variants during chronic infection, often just one R5 HIV-1 is transmitted.
“Understanding how the first cell is infected upon HIV-1 transmission could help inform host susceptibility to HIV-1 and new ways to prevent transmission altogether. Moreover, SLC35A2 is the first host protein that we are aware of that impacts HIV-1 differently based on coreceptor use. Detailing the interactions between host sugars and HIV-1 could shed light on fundamental aspects of HIV-1 entry into host cells.” Looking forward, Itell and Overbaugh remark, “Our findings on SLC35A2 spur two new important routes of investigation for us: mechanism and in vivo relevance. How exactly do SLC35A2 expression and host sugars differentially impact R5 and X4 HIV-1? And do R5 viruses actually have the advantage in the cells that are first infected upon HIV-1 transmission, as we would expect based on SLC35A2 expression patterns? These follow-up studies will help us understand how big of an impact SLC35A2 has on HIV-1 transmission and what specific interactions are driving these effects.”
Dr. Overbaugh holds the Endowed Chair for Graduate Education.
The spotlighted work was funded by National Institutes of Health.
Itell, H.L, Guenthoer J., Humes D., Baumgarten N. E., Overbaugh J. (2024). Host cell glycosylation selects for infection with CCR5- versus CXCR4-tropic HIV-1. Nature Microbiology, volume 9, pages 2985–2996, DOI: 10.1038/s41564-024-01806-7.
Fred Hutchinson Cancer Center
Fred Hutchinson Cancer Center unites innovative research and compassionate care to prevent and eliminate cancer and infectious disease. We’re driven by the urgency of our patients, the hope of our community and our passion for discovery to pursue scientific breakthroughs and healthier lives for every person in every community.
Our values are grounded in and expressed through the principles of diversity, equity and inclusion (DEI). Our mission is directly tied to the humanity, dignity and inherent value of each employee, patient, community member and supporter. Our actions are driven by the commitments expressed in our values: Collaboration, Compassion, Determination, Excellence, Innovation, Integrity and Respect.
Fred Hutch is an independent, nonprofit organization, that also serves as UW Medicine’s cancer program. This unique relationship allows for enhanced care coordination with one of the world's leading integrated health systems .www.fredhutch.org
Contact:
Claire Hudson
She/Her/Hers
Senior Communications Manager
Marketing & Communications
Fred Hutchinson Cancer Center
M 206.919.8300
crhudson@fredhutch.org
Source: Fred Hutch Cancer Centerhttps://www.fredhutch.org/en/news/spotlight/2024/11/overbaugh-x4-r5-tropism-hiv.html
"Reproduced with permission - Fred Hutchinson Cancer Center"
Fred Hutchinson Cancer Center
For more HIV and AIDS News visit...
Positively Positive - Living with HIV/AIDS:
HIV/AIDS News
|