By Joseph Caputo
February 18, 2025
Transmission electron micrograph of HIV-1 virus particles (teal) exiting an infected immune cell after replicating inside the cell. Inset: Interior view a HIV-1 virus showing the capsid (yellow) that surrounds the RNA and enzymes necessary for replication. Credit: National Institute of Allergy and Infectious Diseases
In parts of the world where traveling to a clinic for routine blood tests is a financial and logistical challenge, HIV patients increasingly have the option to collect and ship a drop of their blood in paper-based devices that absorb the sample and store it for analysis in far-away labs.
While this technology is helpful for tracking someone’s adherence to their drug regimen or monitoring disease progression, the most frequently used devices don’t control how much blood they collect, potentially leading to inaccurate readings of a person’s infection.
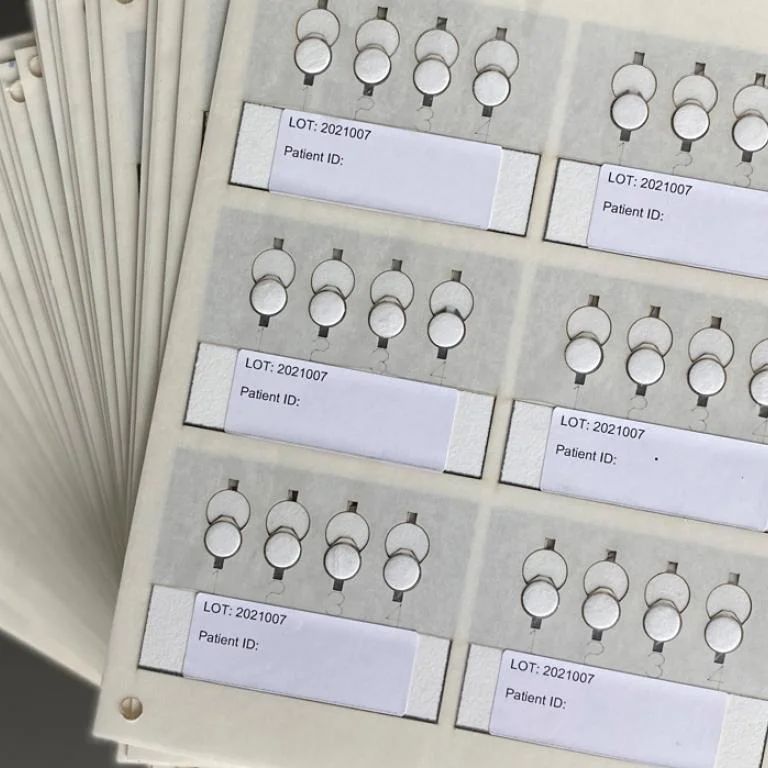
Understanding this limitation, Charlie Mace, an associate professor at Tufts University’s Department of Chemistry, postdoctoral scholar Giorgio Morbioli, and colleagues engineered a paper device with wax-printed patterns that create precise channels and collection spots, ensuring it consistently collects the same volume of blood.
In a clinical pilot with 75 South African patients living with HIV, the Tufts research team’s device, called a plasma spot card, more accurately measured the extent of a patient’s HIV infection versus the industry gold standard, the Roche plasma spot card (90.5% vs. 82.7%) and was better at detecting drug resistant viral mutations (63% vs. 42%), which can influence a physician’s decision to keep someone on the same regimen or switch medications.
Mace’s team reported their findings February 18 in the Proceedings of the National Academy of Sciences.
“Our intuition told us that, because paper will have a defined saturation volume for a unit of area, by patterning a spot with a specific size and shape, we should be able to predict how much plasma it collects,” said Mace, the study’s senior author. “Our cards also needed to be compatible with current workflows to prevent resistance to adoption.”
To conduct the pilot, Mace—with an introduction from HIV experts Michael Jordan and Alice Tang at Tufts University School of Medicine—partnered with the National Institute for Communicable Diseases (NICD) in Johannesburg, South Africa, a major center for disease surveillance, diagnostics, and public health research. NICD scientists provided real-world insights and allowed Tufts researchers to compare the plasma spot cards in a clinical setting where they would be actively used.
Mace is now exploring opportunities to move the technology into regular practice through partnerships with laboratories and researchers both in the United States and internationally. His lab continues to iterate on the device to enhance its accuracy and capabilities while pursuing steps toward commercialization.
“We intentionally focus on developing technologies that are simple, both in construction and operation,” said Mace. “Those kinds of restrictions can make research more difficult, but ultimately we believe in that approach, because simplicity should lead to accessibility and affordability, which are both clearly needed in health care.”
Contact
Kalimah Knight
Kalimah.Knight@tufts.edu
Tufts University
Source: Tufts Now - Tufts University
https://now.tufts.edu/2025/02/18/new-paper-based-device-boosts-hiv-test-accuracy-dried-blood-samples
"Reproduced with permission - Tufts University"
Tufts University
Back to ...
Positively Positive - Living with HIV/AIDS:
HIV/AIDS News
For more HIV and AIDS News visit...
Positively Positive - Living with HIV/AIDS: HIV/AIDS News Archive