|
 October 5, 2011 - In the
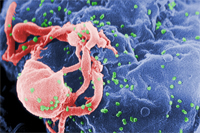
mid-1990s, the widespread introduction of modern antiretroviral therapies changed
a diagnosis of human immunodeficiency virus (HIV)
infection from a rapid death sentence to a chronic condition that could be managed over decades. But as the first generation
of patients receiving these therapies enters late middle age, new challenges are appearing, including a dramatic increase
in the incidence of cancers that were not traditionally viewed as acquired immunodeficiency syndrome (AIDS)-associated
malignancies. October 5, 2011 - In the
mid-1990s, the widespread introduction of modern antiretroviral therapies changed
a diagnosis of human immunodeficiency virus (HIV)
infection from a rapid death sentence to a chronic condition that could be managed over decades. But as the first generation
of patients receiving these therapies enters late middle age, new challenges are appearing, including a dramatic increase
in the incidence of cancers that were not traditionally viewed as acquired immunodeficiency syndrome (AIDS)-associated
malignancies.
Several types of cancer were seen frequently in the early years of the AIDS epidemic; three
types- Kaposi sarcoma , non-Hodgkin lymphoma , and
cervical cancer -are called the "AIDS-defining cancers." A diagnosis of
one of these three cancers can mark the point where HIV infection has progressed to full-blown AIDS.
Researchers tracking the relationship between HIV and cancer over the decades have noticed a substantial
shift in cancer epidemiology in HIV/AIDS patients. In
April of this year, investigators from NCI's Division of Cancer Epidemiology
and Genetics (DCEG) reported in the
Journal of the National Cancer Institute that from 1991 to 2005, even with a quadrupling of the HIV-positive population
in the United States, the number of AIDS-defining cancers diagnosed in that population had fallen by more than two-thirds.
In contrast, the number of non-AIDS-defining cancers had tripled, with the highest number of these new cases
coming from anal , liver , prostate , and
lung cancers and Hodgkin lymphoma . "A big part
of it is that patients with HIV are getting older, and many types of cancer just become more common as people age," said Dr. Eric Engels,
senior author of the DCEG study.
"The HIV-positive population also has a lot of other risk factors for cancer, and that's also contributing," he
added. These risk factors include co-infection with other cancer-causing viruses such as the human papillomavirus (HPV,
which causes cervical, anal, oropharyngeal , and other cancers)
and the hepatitis C virus (HCV, which causes liver cancer),
a high rate of smoking, and possibly the long-term effects of HIV itself on the immune system.
Clinical Trials Conundrum
The increase in HIV-positive patients requiring treatment for non-AIDS-defining malignancies presents a new conundrum: how to provide
the best and safest treatments when data from clinical trials are lacking for these patients. "Traditionally, HIV-positive
patients were de facto excluded from NCI-sponsored clinical trials, except those targeted to AIDS-defining malignancies
like Kaposi sarcoma," said Dr. Robert Yarchoan, director of NCI's Office of HIV and AIDS Malignancy (OHAM).
This exclusion was not based on discrimination, but rather reflected AIDS patients' high susceptibility to drug toxicity, resulting from their profound immunodeficiency.
Also, because they were at risk of death from AIDS, they would confound survival results, Dr. Yarchoan explained.
These concerns are now being reevaluated. The development of highly active antiretroviral therapy (HAART, also known as
combination antiretroviral therapy) has converted HIV infection to a chronic, manageable disease in most cases, and such patients can
now better tolerate chemotherapy. However, a lingering concern is the potential for unknown pharmacokinetic interactions
between the antiviral treatments used to keep HIV under control and cancer chemotherapy drugs or newer biological therapies.
Five years ago, to address the changing pattern of cancers in HIV-infected patients, the NCI-sponsored AIDS Malignancy Consortium (AMC, which spun
off from the National Institute of Allergy and Infectious Diseases' AIDS Clinical Trials Group in 1995) created
a new working group on non-AIDS-defining cancers. "We felt [cancer] was becoming a bigger part of the AIDS epidemic, and we needed
to have a way of testing new drugs in these cancers," said Dr. Ronald Mitsuyasu, director of the AMC and the Center for Clinical
AIDS Research and Education at the University of California, Los Angeles.
The consortium has finished its first safety trial, looking at sunitinib in HIV-positive
patients whose cancers have not responded to standard treatments. It has other such trials in development, testing a variety of newer
treatments including vorinostat , erlotinib , and
other targeted drugs. "Once we've defined that we can safely give a drug and how to give it, any NCI-sponsored trials of these drugs
that excludes patients with HIV will be amended to allow individuals with HIV to enroll, assuming there's no other medical reason they
shouldn't participate," explained Dr. Richard Little, who leads HIV research in NCI's Cancer Therapy Evaluation Program (CTEP) .
"We're trying to make physicians more comfortable with enrolling HIV patients in general oncology trials, so that [HIV status] won't be an automatic exclusion in the
future," said Dr. Mitsuyasu. "Patients with HIV need access to these trials just as much as anyone else does."
In a related effort, CTEP has funded the Blood and Marrow Transplant Clinical Trials Network to perform
two clinical trials in HIV-positive patients, one of autologous bone marrow transplantation,
and one of allogeneic transplantation . "Assuming that
these studies indicate that it is feasible and safe to transplant HIV-positive patients for their underlying cancer, trials that
currently exclude them based on concerns that this is not safe would be amended," explained Dr. Little.
Once we've defined that we can safely give a drug and how to give it, any NCI-sponsored trials of these drugs that exclude patients with HIV will be amended to allow individuals with HIV to enroll, assuming there's no other medical reason they shouldn't participate.
-Dr. Richard Little
"I think the culture is actually changing as people are thinking more appropriately about why patients with
HIV should be included or excluded," he continued. "We're trying to create a culture where the first idea is, yes,
they should be included on a trial unless there's a specific reason that would make that unsafe. People in the research
community are being very responsive to that way of approaching patients."
Increasing Visibility
In the early days of the AIDS epidemic, patients with HIV changed the clinical trials process in the United States, demanding rapid
access to investigational drugs and encouraging community participation. Today, "people don't volunteer like they
used to," said Dr. James Weihe, a psychiatrist who worked on the first AIDS unit at San Francisco General
Hospital back in the early 1980s and now works as an advocate and community representative for the AMC.
"You saw all your friends dying around you, so people were motivated" to participate in clinical trials, he
remembered. "In 1988, you walked down the street in San Francisco and you saw people with Kaposi sarcoma, you saw young people
using canes and walkers and wheelchairs. You don't see that anymore-people look healthy, and the disease has become more invisible."
In addition, even though non-AIDS-defining cancers are becoming more common in people with HIV, "cancer is still
relatively rare-people don't know about [the risk], and they don't necessarily talk to each other about cancer, like they would
for antiviral trials," he continued.
Since most people are referred to cancer clinical trials by their doctors, Dr. Weihe believes it is important to raise
awareness among doctors about cancer trials for HIV-positive patients. "A lot of people don't even know the AMC exists," and
outside big cities and academic centers, "a lot of doctors aren't going to have a large HIV caseload. It's especially important
for us to work with community physicians, because that's where most patients are going."
Drs. Weihe and Mitsuyasu are excited about a new cancer prevention trial the AMC hopes to launch, which will look at
whether anoscopy (an examination of the anal canal) and removal of abnormal tissue can prevent progression to anal cancer, similar
to how the Pap smear and treatment of early
cervical lesions can prevent the
development of cervical cancer. (Both of those cancers are caused by HPV.) "I think the community
might get more involved in this sort of trial-trying to prevent cancer," said Dr. Weihe.
The shift from people with HIV getting cancers at an early age to them getting other cancers at a later age is evidence
of the public health benefit of better treatments for HIV, concluded Dr. Yarchoan. "Instead of people dying of lymphoma (or AIDS)
at the age of 30, they might possibly get lung cancer at the age of 55 or 60. They have many more years without cancer, if they
develop it at all. That's a real development that sometimes gets lost in the story," he said.
- Sharon Reynolds
###
Source: National Cancer Institute
http://www.cancer.gov/ncicancerbulletin/100411/page7
|